When a hot, burning sensation rises from your stomach, spreads to your chest, and even reaches your throat, it can be incredibly uncomfortable. Persistent heartburn and chest pain feel like being burned by the sun, sometimes accompanied by sore throat, coughing, and vomiting, leaving you restless and uneasy.
This discomfort is known as acid reflux and heartburn. Frequent episodes of heartburn often point to Gastroesophageal Reflux Disease (GERD), a common condition, especially in older adults, which causes a lot of discomfort in daily life. We need to update our understanding and scientifically approach the issue of acid reflux, recognizing the disease in time. If you often experience acid reflux, here are four common misconceptions.
Myth 1: Acid reflux means there is too much stomach acid.
The cause is not always excess acid but a problem with the valve between the stomach and esophagus. This “door” doesn’t close properly, allowing stomach contents to flow backward into the esophagus, causing harm. It can result from short-term openings due to alcohol or coffee consumption, or it can be a consequence of aging, where the muscle strength declines and the valve relaxes repeatedly.
While we can’t easily strengthen the valve, stomach contents are mainly acidic. Therefore, reducing stomach acid is necessary to alleviate the impact of stomach fluids on the esophagus. In rare cases, the reflux may not be acidic, and treatment would be adjusted accordingly.

Myth 2: All acid reflux is Gastroesophageal Reflux Disease (GERD).
GERD refers to chronic acid reflux. If you experience occasional acid reflux or it only occurs under certain conditions, it cannot be classified as GERD. You only need to use medication temporarily during episodes or avoid triggering factors, rather than relying on long-term medication.
Additionally, some people may experience heartburn without actual stomach reflux, but due to heightened sensitivity of the esophagus, which overreacts to normal, occasional reflux. In such cases, acid-suppressing medication is not appropriate.

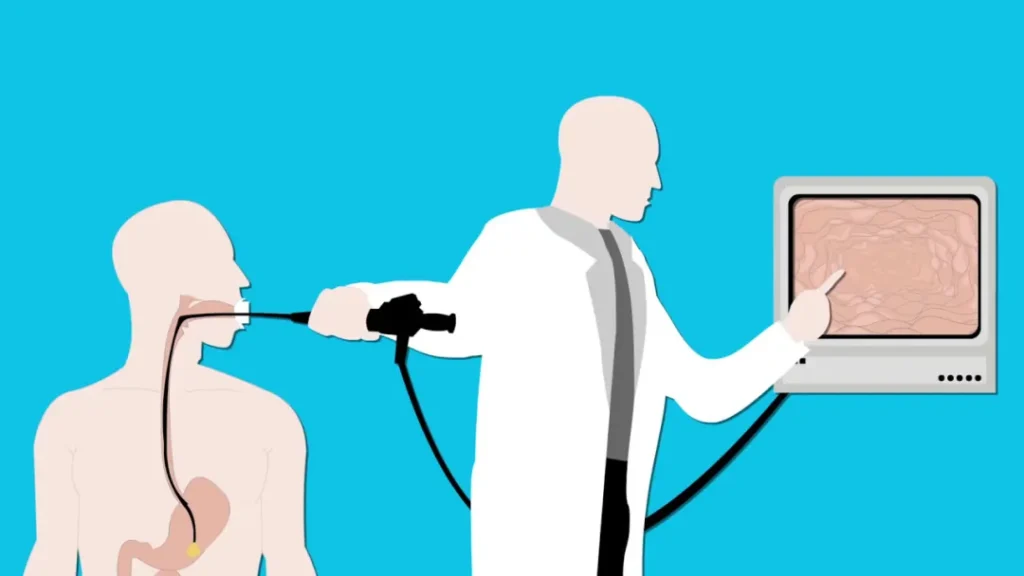
Myth 3: You need a gastroscopy to diagnose acid reflux.
While GERD causes damage to the esophagus, this damage usually occurs at the cellular level and may not be visible during a gastroscopy. Many GERD patients have normal results, with only a few showing typical esophageal erosion. Furthermore, esophageal inflammation may have causes other than reflux disease.
Gastroscopy is recommended to rule out serious conditions, not necessarily to confirm “reflux disease.” GERD can usually be diagnosed through long-term symptoms of heartburn. If symptoms are atypical or treatment isn’t effective, esophageal pH monitoring may be necessary.
Myth 4: You can’t drink coffee if you have acid reflux.
Occasional acid reflux can often be triggered by certain foods, such as coffee, chocolate, alcohol, and sweets. If drinking coffee or eating certain foods causes discomfort, it is fine to temporarily avoid them. However, the main cause of long-term acid reflux is not food. Any food could trigger symptoms, and individual differences vary, so it’s not recommended to avoid coffee unless clearly linked to symptoms.
Keep a food diary to identify foods that trigger reflux, and only limit them if necessary.

Gut Diseases Can Be Confused with Each Other
Many gastrointestinal diseases have similar symptoms, such as functional dyspepsia, stomach ulcers, and duodenal ulcers, which can confuse diagnosis. Misdiagnosing diseases can be more harmful than not treating them at all.

When experiencing gastrointestinal discomfort, don’t make self-diagnoses. It’s important to rule out other potential causes of digestive issues and prevent delays in treatment. If your stomach frequently experiences acid, bloating, pain, or cramps, it’s recommended to consult a doctor. By thoroughly describing your symptoms, a professional doctor can analyze the causes and provide appropriate treatment recommendations.
- When did the discomfort start?
- Which area feels uncomfortable? Upper abdomen or lower abdomen?
- Are you taking medications that may harm the stomach?
- What does the discomfort feel like? Is it bloating or dull pain? Does it occur before or after meals?
- Have you had any previous diseases? Does anyone in your family have hereditary conditions?
- Have you taken any medications for this discomfort? How effective were they? What were the results of previous tests?
Consulting a doctor promptly can save you time and money, and help you achieve better gut health.



















